Neurological Conditions

Autism
What is Autism?
Autism is a childhood neuro-developmental disorder that results from dysfunction in the neurological network of the brain which manifests into the spectrum of autism. Children with Autism shows problems in understanding, thinking abilities, speech, social interactions and behavior. This slows down their normal functioning making them dependent on the near ones. Children with autism need special attention.
The cause of autism has always been debatable and cannot be credited to a single known cause. There are some excerpts brought forward by doctors, researchers and scientists which are mentioned below:
- A structural or a functional damage to the nervous system can produce autism.
- A change in the structure of a gene, often called as a mutation can be responsible for abnormal brain development leading to autistic features.
- Alternatively, non genetic factors like certain perinatal complications such as maternal bleeding in between three months into pregnancy, presence of meconium in the amniotic fluid, insufficient nutrient intake during pregnancy etc.
- Environmental factors (mercury poisoning, maternal stress and exposure to strong medications, toxins, infections or radiations) may also be responsible for autism.
It is essential to realize that no particular individual or event can be held responsible for the child’s diagnosis. Investing in the child’s care and treatment can go milestones in helping a child with autism.

- Increased hyperactivity
- Impulsive behavior
- Short attention span
- Self-injurious behavior
- Aggressive behavior
- Mood swings
- Lack of fear or safety consciousness
- Odd sleep and food habits
Autism assessment requires a team of professionals to evaluate the child at several levels. These include:
- Developmental Pediatrician
- Clinical psychologist
- Occupational therapist
- Speech and Language pathologist
- Neuroimaging Studies
- Magnetic Resonance Imaging (MRI)
- Computed Tomography (CT)
- Positron Emission Tomography- Computed Tomography (PET- CT scan)
- Electroencephalography (EEG)
- Brain stem evoked response audiometry (BERA)
Autism is incurable and requires chronic management. At present treatment for autism can be divided into below interventions:
- Medical management
- Occupational Therapy
- Psychological Intervention
- Speech Therapy
- Physiotherapy
- Diet and Nutrition
- Art, Play, Music and Dance Therapy
- Animal Assisted Therapy
Recent data has indicated that early intensive rehabilitation therapies can considerably improve the symptoms of children with Autism. Such therapies can be designed to provide development and learning, promoting socialization, self-awareness, reducing maladaptive behavior and educating supporting families.
Daily rehabilitation programs help to integrate child back into society comprise of below therapies:
- Psychological intervention
- ABA therapy
- Occupational therapy
- Sensory integration
- Physiotherapy
- Speech Therapy
- Special education
- Art & Music therapy
- Dance therapy
- Aquatic therapy
- Diet & Nutritional intervention
Nutritional interventions restrict allergy-associated dietary components and supplement minerals or vitamins that are lacking. Autistic children tend to have problems with digestion, including food sensitivity – particularly to casein and gluten in dairy and wheat products.
The Rehabilitation strategies help in the management of associated symptoms and improving the physical and cognitive abilities, restoring the patient to daily life.
Children with Autism have shown improvements in below areas following rehabilitation therapies:
- Attention and concentration
- Cognition and learning
- Speech and communication
- Command following
- Activities pf daily living (ADL)
- Hyperactivity
- Eye Contact
- Social interaction
- Communication
- Behavior
- Problem solving
- Alertness
- Physical activities
- Balance and posture

Cerebral Palsy
What is Cerebral Palsy?
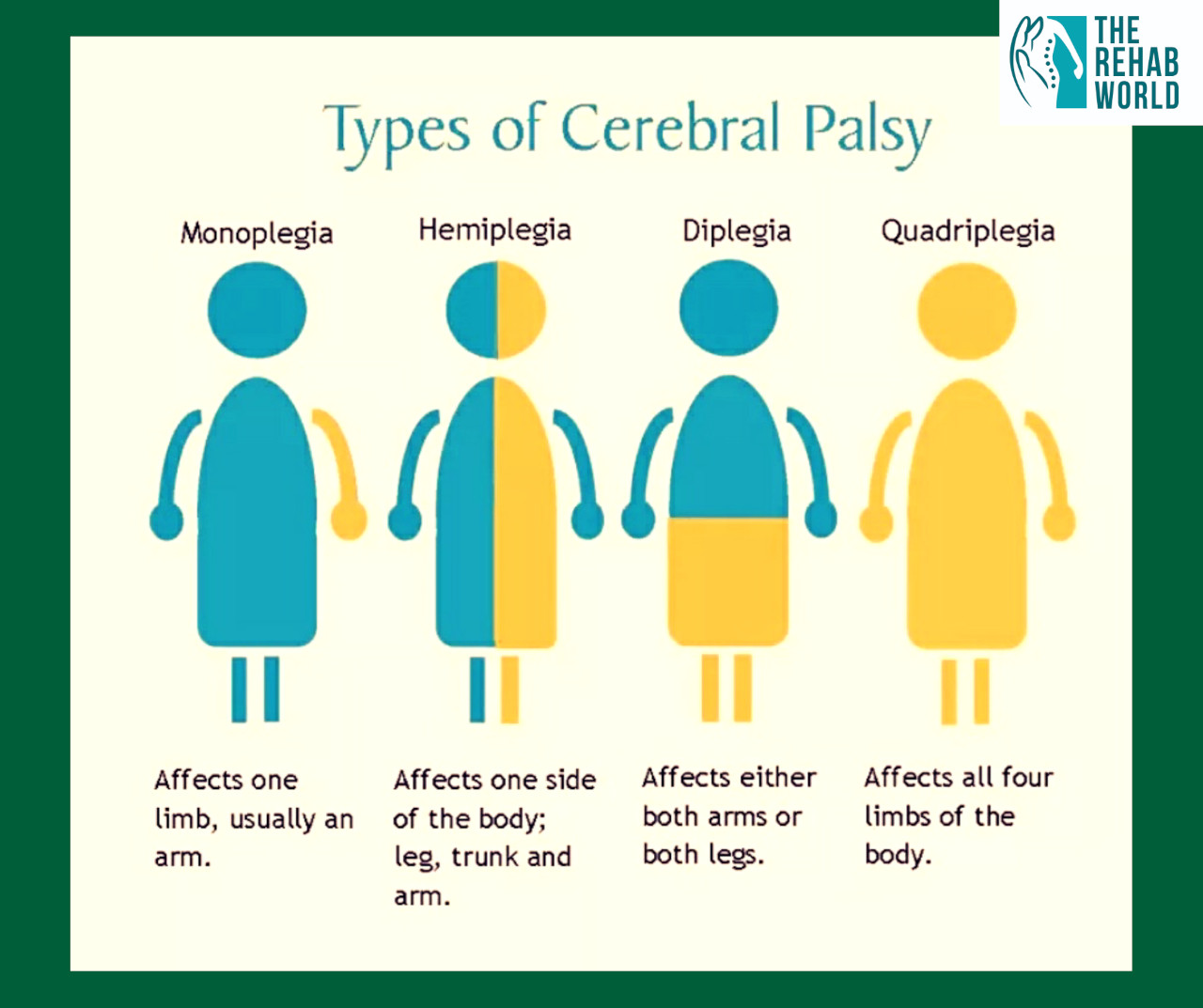
Cerebral Palsy is considered a neurological disorder caused by a non-progressive brain injury or malformation that occurs while the child’s brain is under development. It is an abnormality of motor function (as opposed to mental function) and postural tone that is acquired at an early age, even before birth. Cerebral Palsy affects approximately one to three out of every thousand children born. However, it is much higher in infants born with very low weight and in premature infants.
- Reduced oxygen supply to the brain during the birth of the child, which may be caused as a result of the cord stuck around the neck.
- Infections during pregnancy or physical injury can cause damage to the brain.
- Complications of premature birth.
- Critical illness at birth (neonatal encephalopathy) that decreases the supply of oxygen to the brain.
- Development of the brain in an unusual shape or structure.
- Genetic mutations in the brain cell that affect brain development.
- Lack of muscle coordination when performing voluntary movement
- Stiff or tight muscles and exaggerated reflexes (spasticity)
- Weakness in one or more arm or leg
- Walking on the toes, a crouched gait, or a “scissor” gait
- Variations in muscle tone, either too stiff or too floppy
- Excessive drooling or difficulties swallowing or speaking
- Shaking (tremor) or random involuntary movements
- Delays in reaching motor skill milestones
- Difficulty with precise movements such as writing or buttoning a shirt.
Most children with Cerebral Palsy are diagnosed during the first 2 years of life. But if a child’s symptoms are mild, it can be difficult for a doctor to make a reliable diagnosis before the age of 4 or 5.
Below tests can be done to diagnose Cerebral Palsy
- Routine lab blood and urine tests
- NeuroImaging techniques:
- Cranial ultrasound
- Positron Emission Tomography – Computed tomography (PET-CT)
- Magnetic resonance imaging (MRI)
- Electroencephalogram
- Medications
- Physiotherapy
- Occupational therapy
- Surgical aids
- Mobility aids
- Psychology/Neuropsychological assessment
Below improvements were noted after intensive rehabilitation in children with cerebral palsy
- Improvement in standing
- Improvement in sitting tolerance
- Improved stamina
- Improved respiratory capacity
- Louder and clearer speech
- Improvement in shoulder movements
- Improvement in shoulder strength
- Improvement in sitting balance
- Can walk with support of splints

Muscular Dystrophy
What is Muscular Dystrophy?
Muscular Dystrophy refers to a set of more than 30 genetic diseases that causes progressive weakness and degeneration of skeletal muscles used during controlled movement. These problems differ in an era of onset, severity and an outline of affected muscles. All types of muscular dystrophy grow worse as muscles increasingly deteriorate and weaken.
Muscular dystrophy is a neuromuscular disease characterized by progressive muscle weakness, degeneration and necrosis. Some of the causes are as below:
- Mutation in the dystrophin gene
- Absence of essential muscle protein dystrophin
- Progressive muscle degeneration
- No definitive medical or surgical treatment available
- Progressive deterioration
- Ventilator and death
Muscular dystrophies are a set of inherited disorders that disrupts the functioning of one out of thousands of genes that produces the dystrophin protein necessary for maintaining muscle integrity.
This means that the cells that preserve the muscle integrity can no longer serve its purpose leading to progressive muscle weakening and disability. Many muscular dystrophy’s occur through unprompted changes in the gene structure and then those flaws can also be transferred from one generation to the other. Muscular dystrophy can be inherited in three ways:
- Autosomal dominant: This inheritance occurs when a child receives a defective gene from one parent and a normal gene from the other parent.
- Autosomal recessive: This inheritance means that both parents must bear and pass on the defective gene. It means that both the parents must possess one defective gene but remain unchanged by the disorder.
- X-linked recessive: When a mother carries the affected gene on one of her two X chromosomes and passes it to her son, then the X-linked (or sex-linked) recessive inheritance occurs.

- Duchene muscular dystrophy
- Becker muscular dystrophy
- Congenital muscular dystrophy
- Distal muscular dystrophy
- Emery- Dreyfuss muscular dystrophy
- Limb-Girdle muscular dystrophy
- Facioscapulohumeral muscular dystrophy
- Myotonic muscular dystrophy
- Oculopharnyngeal muscular dystrophy
Muscular Dystrophy is characterized by general weakness, wasting of muscles, difficulty in walking or limb function. The signs & symptoms of Muscular Dystrophy vary from types to type.
- Duchenne Muscular Dystrophy: Frequent falls, difficulty in climbing stairs, walking on toes. waddling gait, running, jumping and getting up from squatting position. It also leads to learning disabilities, delayed growth and weakening of heart.
- Becker’s Muscular Dystrophy: Similar to DMD but tend to be milder and progress slowly. It leads to skeletal deformities of spine and chest and also affects the heart muscle.
- Congenital Muscular Dystrophy: Primarily affects the voluntary muscles and joints. Delayed motor milestone, intellectual or learning disabilities, possible seizures and vision defects. Weakness of the brain and eyes which leads to deformed spinal curvature and respiratory deficit.
- Distal Muscular Dystrophy: Weakness of distal muscles, i.e., the lower arms and legs and gradually extents to other parts of the body.
- Emery-dreifuss Muscular Dystrophy: Joint deformities and contractures, muscle wasting and weakness.
- Limb-Girdle Muscular Dystrophy: Muscle wastage and weakness especially of hip and shoulder.
- Facioscapulohumeral Muscular Dystrophy: Prolonged muscle contractions, temporarily locked jaw, slurred speech, cramping of the hands after use. It tends to affect face, feet, hands and neck.
- Oculopharyngeal Muscular Dystrophy: Drooping eyelids and difficulty in swallowing eventually leads to severe lack of nutrition.
- Clinical Examination
- CPK levels
- Muscle Biopsy
- Electromyogram
- Genetic Testing
- Magnetic Resonance imaging
Muscular dystrophy is one of the toughest disorders to treat. The pathogenesis is known but yet there is no cure to any form of the condition.
Current treatment available for Muscular Dystrophy are focused on limiting the degenerative effects, some of them are as below:
- Medical treatment of complications: Medication usually consisted of corticosteroids that aided in muscle regeneration or alternatively, steroids were used to inhibit the degeneration of muscles.
- Surgical Management of Contractures & Deformities.
- Gene Therapy: aimed at normalizing the protein production and rooting out the very cause of condition.
- Rehabilitation: Physiotherapy, Occupational therapy, Speech therapy, Psychological counselling, Cardiorespiratory Rehabilitation, Diet & Nutrition that helps the patient lead a more complete and independent life.
Rehabilitation aims as improving muscle strength, aerobic capacity, independence and prevent deformities.
Some of the improvements seen post rehabilitation are as below:
- Improved trunk strength
- Improved upper limb strength
- Improved lower limb strength
- Gait improved
- Improved sit to stand

Spinal Cord Injury
What is Spinal Cord Injury?
Any damage to the cord due to trauma, loss of blood supply or infection resulting in loss of normal motor, sensory or autonomic functions.

- Based on Cause
- Traumatic injury
- Non-Traumatic injury
- Based on Severity
- Complete injury
- Incomplete injury
- Cervical injury
- Dorsal injury
- Lumbosacral injury
A patient with Spinal Cord Injury might display the following characteristic signs:
- Trouble with walking and proper movement
- Inability to differentiate sensations and feel heat, cold and touch
- Loss of the control of the bowel or bladder movements
- Moments of inflated reflex actions
- Unnatural sexual function and sensitivity
- Moments of growing numbness and tingling to extreme
- Signs of breathing problems and coughing
Investigations that can be carried out to diagnose Spinal cord injury are:
- X-Ray: Shows fracture or damage to spine
- MRI: Shows location and extent of damage
- F-MRI: Helps in measuring activity in brain and Spinal cord
- CT Scan: Cost effective highly sensitive for detection of spinal fracture
- SSEP: Somatosensory evoked potential-shows if nerve signals can pass through the spinal cords.
- Deep vein thrombosis
- Urinary tract infection
- Postural Hypotension
- Heterotrophic Ossificans
- Bedsore
- Osteoporosis
- Autonomic Dysreflexia
- Emergency Care
- Medication
- Immobilization
- Surgical Management
- Rehabilitation
Rehabilitation for Cervical level injury includes:
- Bed Mobility
- Hand Rehabilitation
- Wheelchair Mobilization
- ADL Training
- Transfer Training
- Standing
- Fine Motor Training
- Psychology Counseling
Rehabilitation for Dorso-lumbar Injury
- Balance training
- FRO Gait Training
- Gait Training with KAFO
- Kunming Therapy
- Psychology Counseling
- Transfer Training
- Vocational Training
- Wheelchair Sports
Symptomatic improvements seen in Spinal Cord Injury patients post intensive rehabilitations are:
- Spasticity
- Sensation
- Bladder Sensation
- Upper Limb Strength
- Sitting Balance
- Standing Balance
- Walking Balance
- Trunk Stability
- Trunk muscle strength
- Postural Hypotension

Brain Stroke
What is Brain Stroke?
Brain stroke also known as Cerebrovascular accident happens when the blood and oxygen supply reduces or gets interrupted from reaching the part of the brain tissue because of blockage or a bleed. Rapidly developing clinical signs of focal (or global) disturbance of cerebral function with symptoms lasting 24 hours or longer or leading to death with no apparent cause other than of vascular origin. Without oxygen, brain cells and tissues gets damaged and begin to die within minutes, that’s why early intervention is important and essential to reduce brain damage and other complications which ultimately result in brain stroke. Although men have more chances to have stroke in their younger years than women, it has been noted that women have a higher lifetime risk of having a brain stroke than men.
Stroke can be classified in 3 types:
Ischemic stroke: Most common type of stroke which happens when the blood vessels supplying to a particular part of the brain gets blocked resulting in severely reduced blood flow (ischemia). Ischemic stroke is of 3 types
- Thrombotic stroke: happens when a blood clot forms in one of the arteries supplying blood to brain. This clot passes through the bloodstream and becomes lodged in the narrow arteries blocking the blood supply to that particular part of the brain.
- Haemorrhagic stroke: occurs when an artery in the brain bursts open and leaks blood creating excess pressure in the skull and results in swelling, damaging surrounding brain tissue.
- Transient ischemic attack: also known as ministroke, occurs when blood supply to the brain gets temporarily blocked by a clot or a debris.
There are several risk factors involved which lead to brain stroke, some of them are modifiable like high blood pressure, diabetes if managed properly and some of them are non modifiable as it is not in anyone’s control like age.
- Non-Modifiable
- Age
- Gender
- Race
- Genetic
- Modifiable
- High Blood pressure
- Blood Cholesterol
- Diabetes
- Heart Disease
- Cigarette Smoking
- Alcohol Intake
- Sedentary Lifestyle
- Obesity
- Stress
Several measures can be taken to prevent or delay stroke, specially if followed a proper lifestyle and diet. Some of them are mentioned below:
- Keep your blood pressure low
- Lower your cholesterol
- Eat healthy food
- Exercise regularly
- Treat sleep apnea
- Manage your diabetes
- Drink in moderation
- Stop smoking
- Avoid stress
- Maintain healthy weight
It is important to provide immediate care to apatient suffering from stroke, sooner the person gets care better the outcome will be. Therefore, it is important to understand early signs and symptoms of stroke to take immediate action.
Common symptoms of stroke are as below:
- Weakness of the face, arm or leg on one or both sides of the body.
- Imbalance while sitting or standing
- Ataxia – lack of coordination while doing activities
- Vision problems, such as trouble seeing from one or both eyes, slurred or double vision, blackout.
- Loss of speech, slurred speech, difficulty in talking, or understanding what others are saying.
- Problems associated with hearing
- Sudden, severe headache with unknown cause.
- Confusion, disorientation or lack of responsiveness.
- Fainting or loss of consciousness.
If anyone suffers a stroke, a physician or neurologist would do certain investigations to confirm the diagnosis. Investigations that can be carried out to diagnose brain stroke are:
- Blood Test
- Brain Imaging Test
- Heart and Blood Vessel Test
- Leg Ultrasound
- Electrocardiogram
- Transcranial Doppler
To confirm and advice further course of action for a patient suffering from stroke several assessment needs to be done as below:
- Demographic data
- Vital signs
- History Taking
- Motor Assessment
- Sensory Assessmen
- Cranial Assessment
- Acute care
- First line management: immediate intervention should be taken if a person has suffered a stroke to prevent any further brain damage. Primarily, doctors put a patient under oxygen and keeps them under an intravenous drip to help patients restore or avoid its occurrence in the first place.
- Medication: aim is primarily to prevent a second attack.
- Surgical Management
- Neurorehabilitation
If the brain damage after stroke is irreversible and the patient has sustained disability then a rehabilitation program can be recommended to overcome the damages caused and help in improving the disability and resume daily activities with support.
Rehabilitation therapies that can help a patient suffering from stroke are:
- Physiotherapy
- Occupational therapy
- Speech therapy
- Psychological counselling
- Diet and nutrition program
These therapies are safe and well tolerated and help to improve a patient’s overall well-being. Rehabilitation plays a vital role in restoring the lost strength. The therapies given to patients vary individual to individual and each person’s ability to recover from complications varies widely. To yield a good outcome, rehabilitation should be started as early as possible. Degree of improvements varies from patient to patient.
Post rehabilitation stroke patients shows below improvements:
- Improved upper limb activity
- Improved hand functions
- Better lower limb activity
- Improved trunk activity
- Improved balance
- Improved speech
- Better ambulation
- Better all-day living activity
- Reduced fatigue and depression

Down’s Syndrome
What is Down’s Syndrome?
Down syndrome is a chromosomal disorder that causes impairment in physical and cognitive growth of a child. It is the most common cause of mental retardation. People with Down syndrome present with typical features, such as a flat face and a short neck. These features vary from individual to individual. It is a lifelong condition. But with appropriate care and support, children with Down syndrome can grow up to have healthy and productive life.
Down syndrome is caused by a presence of extra chromosome 21. Chromosomes carry the genes that instruct the body to develop in certain ways and to perform certain functions. Most cells of the human body contain 23 pairs of chromosomes, one set of chromosomes from each parent. People with Down syndrome have 47 chromosomes. In rare cases, other chromosome problems can also cause Down syndrome. Having an extra or abnormal chromosome disrupts the normal course of development and results in the physical features and intellectual and developmental disabilities associated with the syndrome.
The most common symptoms seen in children with Down syndrome are:
- Distinctive facial features, such as a flat face, small ears, slanting eyes, short neck, arm and legs and small mouth
- Single, deep creases across the center of the palm
- A single flexion furrow of the fifth finger
- Lower muscle tone and loose joints
- Below-average intelligence
Moreover, children with Down syndrome are also born with heart, intestine, ear, or breathing problems. These conditions often lead to other complications, such as airway infections or hearing loss.
Currently, there is no standard treatment available for Down syndrome. Different treatment strategies are available based on the child’s physical and cognitive needs and limitations. These include:
Physiotherapy: include exercises and activities that aim at improving the muscle strength, posture and balance.
Speech-language therapy: Exercises and activities that aim at improving the communication skills, speech impairments and language understanding. This helps the children with the syndrome to effectively communicate with the peers in school and home.
Occupational therapy– Helps the child to develop skills for activities of daily living and lead a good quality of life. This includes self-care skills like bathing, dressing, eating, etc.
Behavioral therapy– These activities aim at understanding the compulsive behaviors in the patients and using creative strategies to prevent these behavioral responses.
Drugs and Supplements– These include amino acid derivatives that aim at improving the brain activity. But these supplements have presented with various adverse effects in many clinical trials.
Assistive devices– Intervention with these modified devices enhance the learning and task management abilities in children with Down syndrome.
The main goal of all these treatments is to develop the child’s potential to the best of his/her ability, to integrate them back into society and help to lead a respectable life.
The Rehabilitation strategies help in the management of associated symptoms and improving the physical and cognitive abilities, restoring the patient to daily life.
Child with Down’s syndrome have shown improvements following rehabilitation therapies:
- Attention and concentration
- Memory
- Understanding and communication
- Interest in learning new tasks
- Command following
- Problem solving
- Alertness
- Speech and pronunciation
- Identification and thinking ability
- Physical activities
- Balance and posture
- Activities of daily life (ADL)

Ataxia
What is Ataxia?
Ataxia is a condition where a person lacks coordination during voluntary movement. The cerebellum, which is the main center of the brain to control coordination, is mainly affected during ataxia. Cerebellum is a part of the human brain that controls and coordinates movements. It fine-tunes the signals received from the brain, spinal cord and other structures and delivers a polished result. Although, ataxia can be classified into several types, when the cerebellum is mainly affected, it leads to cerebellar ataxia.
Ataxia occurs when the functioning of the cerebellum gets affected. It leads to uncoordinated voluntary movements and loss of balance. Spinocerebellar ataxia (SCA) is a type of Ataxia that affects the cerebellum, its surrounding structures and its connection to the spine. The most characteristic feature is the walking pattern that mimics the “drunkard’s gait”. In addition, the hand movements, speech and eye movements are also uncoordinated.
There is no definite cause of Cerebellar ataxia, it can be progressive, starting in childhood, teenage, or 3rd or 4th decade of life. Most often, ataxia is associated with atrophy (shrinking) of cerebellum.
Cerebellar ataxia could either be acquired or hereditary in nature.
- Acquired ataxias could occur due to severe head injury, bacterial brain infection such as meningitis, viral infection, cerebral palsy, multiple sclerosis and so on.Hereditary ataxias are caused due to a faulty gene passed down from one generation to the next.
Ataxias could be classified into different types, based on their affection and causes. While the clinical presentations are very similar, the two most common types of ataxias are as follows:
Cerebellar Ataxia – This type of ataxia occurs due to abnormality in the cerebellum.
Spinocerebellar Ataxia – This type of ataxia occurs due to abnormality in the cerebellum as well as spinal cord.
A person suffering from Ataxia face difficulties in all voluntary movement as well as other comorbid factors. Some of these symptoms are:
- Problems with balance
- Poor limb coordination
- Tremors – parts of the body may shake or tremble unintentionally
- Dysarthria – slurred and slow speech
- Swallowing difficulties
- Facial expressions become less apparent
- Walking difficulties
- Vision problems
- Hearing problems
- Depression
- Cold feet – because of a lack of muscle activity
- Medications
- Use of assisted devices such as walkers, canes etc.
- Rehabilitation programs such as physiotherapy, occupational therapy, speech therapy and Psychological counselling.
- Decreased jerky in-coordinated movements
- Less assistance required for walking
- Reduced spasticity
- Improved joint movements and flexibility
- Less titubations
- Improved standing balance
- Improved speech and voice quality
- Reduced tremors during slow and prolonged speech
- Improved respiration
- Relaxed neck and shoulders
- Improved stamina
- Improved oromotor skills

Dementia/Alzheimer's/Parkinson's
What is Dementia?
Dementia is a disorder that cannot be well defined. It results in acute deterioration in the mental capacity which slows down the thinking and social capabilities making it difficult for normal living. It is a group of symptoms that occurs due to some brain disorders. Memory loss is one of the most common symptom of dementia. But not all the cases of memory loss are related with dementia. Dementia can occur when two or more functions of the brain are affected without losing one’s sense like memory, language, reasoning, judgment and so on.
A progressive form of Dementia leads to Alziemer’s disease which destroys memory and other mental functions
In Alziemer’s brain cells which forms all connections degenerates and die resulting in severe memory loss and loss of important mental functions
Parkinson’s is a neurological disorder where central nervous system is damaged which controls movements of the body which eventually results in tremors.
Nerve cells damage results in drop of dopamine level leading to symptoms of Parkinson’s
Any injury to the brain cells can lead to Dementia. Any damage to these brain cells can affect the correspondence between them which affects a person’s normal communication, behavior and thinking abilities.
Dementia can be classified into different types based on its common features. The frequently used classifications are:
Cortical dementia- affects the outer layer (cortex) of the brain
Sub cortical dementia- affects the lower layer of the cortex
Progressive dementia- this condition worsen with time, slowly causing an increased obstruction with cognitive abilities which leads to Alziemer’s disease
Primary dementia- is not a consequence of any other disease
Secondary dementia- caused due to an outcome of a physical injury
Progressive dementia generally occurs in people with Alzheimer’s disease, vascular Dementia and Lewy body dementia. The most common type of progressive dementia is Alzheimer’s disease. Dementia can also occur due to other neurological disorders like Multiple sclerosis, Huntington’s disorder, Traumatic Brain Injury, and Parkinson’s disease. Manh dementias that take place are wavering and visible in the case of immune disorders, metabolic disorders, nutritional deficiency and reactions to certain medications.

Progressive dementia like Alzheimer’s disease and Parkinson’s has no possible cure or treatment that can stop its progression. Though there are some drug treatment options that can momentarily improve the symptoms. Some medications can be given to improvises the cognitive skills of a person momentarily. Most of the dementia symptoms and behavioral problems can be treated primarily with the use of non drug approaches. With the help of rehabilitation therapies such as physiotherapy, occupational therapy & psychological interventions, patients with dementia will be able to deal with changes in behavior and normal daily activities.
- Improved functional and symptomatic behaviour
- Improved emotional response
- Better cooperation
- Reduced crying spells
- Improved sitting tolerance
- Improved memory attention
- Improved concentration
- Improved mathematical abilities and reasoning.
- Improved all day living activities
- Improved oromotor control and swallowing movements
These positive changes are recorded objectively on the neuropsychological test of Mini Mental Status Examination (MMSE).

Other Neurological Conditions
Rehabilitation therapies such as physiotherapy, occupational therapy, speech therapy, psychological counseling, yoga therapy, diet and nutrition can be given to all the above neurological disorders as well as others like head injury, intellectual disability, motor neuron disorder, cerebral atrophy, spino muscular atrophy etc. The aim of rehabilitation therapies is to improve the overall quality of life patients suffering from the above incurable neurological disorders.